To improve point-of-care HCC coding capture among providers, most ACOs and population health teams rely on provider education programs. Successfully developing these programs can be challenging. HCC analytics, when leveraged correctly, can help you optimize provider education, as well as track and measure the impact of these efforts. Many top-performing population health teams have successfully used HCC analytics and reporting from RCxRules HCC Coding Software to shape their educational programs, improve provider capture performance, and track their success in real time.
Getting Started
The first step in creating or modifying a provider education program is establishing a baseline. By gathering data, you can determine which providers are doing well with HCC capture, and which could do better. You might choose to look at a prescribed set of specialties to further focus your efforts. Typically, primary care and internal medicine providers act as the quarterbacks of their patients’ care—they tend to spend more time with their patients, particularly at annual wellness visits—meaning they often have the most opportunities to improve their HCC capture rates. This specialty-specific baseline data will help you identify potential areas for improvement so you can determine your priorities and create action plans.
Leveraging HCC Analytics from the Add/Remove Report
With the flexible reporting capabilities of RCxRules, there is a lot of HCC data available to analyze. When it comes to improving point-of-care capture and provider education, the most commonly used report is the Add/Remove report.
The Add/Remove report displays instances where providers may be doing a great job with documentation, but coder review has revealed their coding could be improved. Specifically, it shows where coders were able to add or remove HCC codes based on supporting provider documentation.
For example, see Provider #1 below. This data shows that a coder found four instances of one provider documenting diabetes without complications where there was, in fact, supporting documentation of complications that the coder used to be more specific in the diagnosis and ensure a more accurate RAF score.
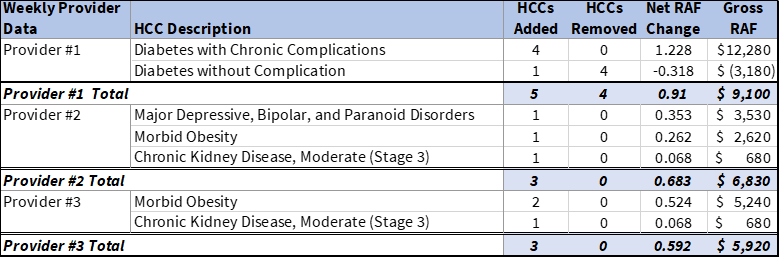
The data on this report can lead to a variety of opportunities to improve provider education and point-of-care HCC capture. Below are some common use cases:
- Provide real-time provider feedback. Using the Add/Remove report, you can engage your providers within a few days of the patient visit in question, while it’s still fresh in their minds.
- Identify HCC coding provider champions within specialties. The providers who excel at documentation and coding make good mentors. Our customers find that physicians are often more open to receiving HCC coding feedback from a peer. Oftentimes this takes place in smaller committee meetings.
- Measure the effectiveness of your training. Monitoring these statistics over time will help you objectively measure how effective your efforts have been. Based on the actions taken, are you seeing improvement? If your group is investing time and money in provider education and point-of-capture mechanisms, it is important to have a system in place to measure results for continual improvement.
How One ACO Used HCC Analytics to Focus their Provider Education Efforts and Improve Risk Adjustment Performance
One ACO we work with, a 100+ provider multispecialty group in the Midwest, was highly focused on providing education to primary care providers. After reviewing their reports from RCxRules, they realized there was an opportunity to shift their education focus to endocrinologists. They conducted refresh training with the endocrinologists to improve documentation and HCC coding, and developed a weekly newsletter to reinforce the important lessons. In the first three months of this program, the improved documentation by their endocrinologists led to HCC coders increasing HCC accuracy in one out of every four claims.
Learn how our HCC coding software and reporting can help guide your provider education efforts, point-of-care capture, and improve risk adjustment performance. Set up a 15-minute meeting to learn more.