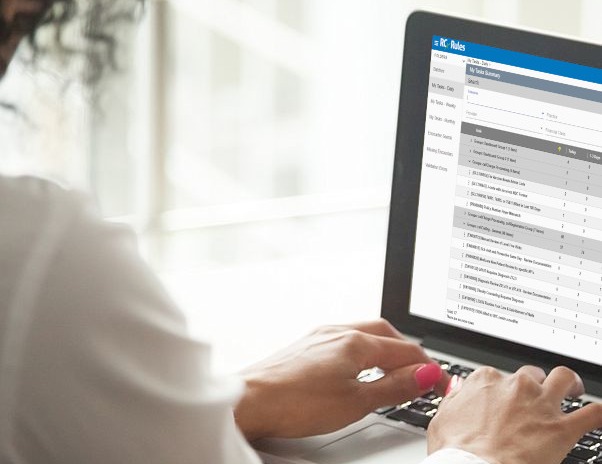
Increase Your RAF Score Accuracy, Not Your Workload
You deserve to be paid for the exceptional care you provide to your patients. This simple and realistic goal is often challenged by the complexities of value-based care. Physicians are experts at patient care, not coding, which inevitably leads to gaps between documentation and HCC coding. These gaps lead to inaccurate RAF scores and decreased revenue. Our AI technology automatically finds encounters that have been well documented but inaccurately coded, so doctors can be doctors—and coders can boost revenue by immediately improving RAF score accuracy.
Trusted by




.png)






Why Choose the HCC Coding Engine?
Our technology reviews every encounter that leaves your EMR in real time. If an encounter does not need coder review, it automatically passes through to your revenue cycle system in milliseconds. If the technology detects an HCC coding gap, it directs the encounter to a coder for review. These changes are integrated back into your revenue cycle system, so accurate claims are sent every time.
"The automation RCxRules brought to our HCC coding process led to a dramatic productivity hike in our organization and is a key factor in our success with MSSP. The technology is extremely user friendly and the RCxRules team is flexible and responsive."

The Future Isn’t Coming, It’s Already Here
The impact of value-based care on the bottom line of medical groups across the country is continuing to grow. We understand the transition to value-based care isn’t easy—and ensuring you have a consistent and predictable revenue stream is a necessity. That’s why we leverage technology to improve HCC code capture and CPT II code capture for quality measures. In both cases, the goal is to close the gap between what the providers document and what gets reported to the insurance companies. Stay a step ahead as the world moves towards value-based care.

Reduce Burden on Providers
Providers went to medical school to become doctors, not coders. They excel at providing patient care, but often struggle to translate the care provided into HCC codes. Provider education is a good place to start—but providers need support to truly improve RAF score accuracy. That’s why our technology works with your coders, so there’s no additional work required from already overburdened providers.

Improve Coder Productivity
Coders have a wealth of specialized knowledge—knowledge that shouldn’t be wasted on reviewing routine encounters. Our pioneering HCC Coding Engine identifies critical, high-value HCC encounters that warrant full coder review, so coders can make the most of their time and skills. The result? A single coder working with our HCC Coding Engine finds at least $250,000 in RAF value every month.

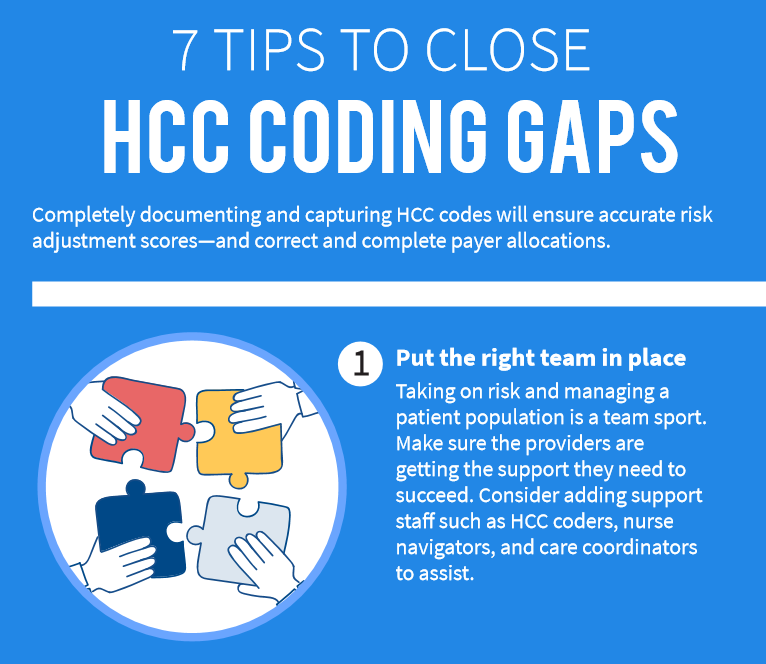
Close the Gap
Physicians are much better at clinical documentation than HCC coding. In fact, 1/3 of encounters flagged by the HCC Coding Engine are underreporting HCC codes when compared to the physician documentation. This means your physicians aren’t getting credit for the documentation they entered and the care they provided. Our HCC Coding Engine automatically identifies these potential gaps and directs them to a coder for review.

-
Reduce Burden on Providers
Providers went to medical school to become doctors, not coders. They excel at providing patient care, but often struggle to translate the care provided into HCC codes. Provider education is a good place to start—but providers need support to truly improve RAF score accuracy. That’s why our technology works with your coders, so there’s no additional work required from already overburdened providers.

-
Improve Coder Productivity
Coders have a wealth of specialized knowledge—knowledge that shouldn’t be wasted on reviewing routine encounters. Our pioneering HCC Coding Engine identifies critical, high-value HCC encounters that warrant full coder review, so coders can make the most of their time and skills. The result? A single coder working with our HCC Coding Engine finds at least $250,000 in RAF value every month.

-
Close the Gap
Physicians are much better at clinical documentation than HCC coding. In fact, 1/3 of encounters flagged by the HCC Coding Engine are underreporting HCC codes when compared to the physician documentation. This means your physicians aren’t getting credit for the documentation they entered and the care they provided. Our HCC Coding Engine automatically identifies these potential gaps and directs them to a coder for review.

How the HCC Coding Engine Benefits Your Organization
CFOS
Generate the revenue required to succeed in value-based contracts by accurately aligning RAF scores with your patients’ health status.
POP HEALTH AND HCC CODING LEADERS
Boost your HCC coders’ productivity by 300%. Automatically identify high-value HCC encounters so your coding team is focused on the visits that have the biggest impact.
PROVIDERS
Get the credit you deserve for providing high quality patient care with no additional work. Align HCC coding with your documentation by leveraging coders and the HCC Coding Engine.
Need Coders? Combine Technology and Talent for the Most Accurate Coding
The AAPC + RCxRules Advanced Coding managed service acts as an HCC coding safety net. This unique approach means you only incur a cost when AAPC-Certified Risk Adjustment Coders deliver results—you only pay when an HCC code is added, deleted, or adjusted. There are no implementation fees or hidden costs.
Learn More