Throughout history, many of the greatest innovations happened either completely by accident or by taking a solution to an old problem and applying it to a new one.
The transition to value-based care has created an abundance of challenges that require innovative solutions. One that continues to grow in importance and urgency is the need to improve HCC coding performance.
Fortunately, you already have a powerful resource in your own organization that can help significantly with HCC coding—and you probably don’t even know it.
We’ll tell you what it is in a moment. But first, let’s look at how an organization in a completely different industry and era dealt with a disruptive change in their revenue model.
Back In 1933, coal was a widely used heating fuel in American homes, and its tendency to deposit a layer of black soot on nearly everything enabled Kutol, a Cincinnati-based manufacturer of wallpaper cleaner, to prosper for about two decades. But by the mid-1950s, consumers were shifting to other sources of heat, and sales were plummeting.
The company’s future looked bleak until a nursery school teacher tried using some of Kutol’s product to make holiday decorations with her class. When the kids had more fun playing with the wallpaper cleaner than they did doing the original project, she contacted the company.
A minor reformulation transformed it into a new product that became a huge hit. And today, over 60 years later, Play-Doh—the perennially popular substance children squish and squeeze into anything they can imagine, from dinosaurs and buildings to misshapen blobs no grownup can identify—is still going strong.
But how is this relevant to HCC Coding?
Well, you already have a “wallpaper cleaner”—i.e., a solution to an older challenge—in your organization that you can “reformulate” to help solve the more recent challenge of HCC coding.
Your revenue cycle team was put in place to help your organization prosper under the classic fee-for-service (FFS) reimbursement model. All day long, these skilled professionals continue to use proven technologies and processes to review every claim BEFORE it ever goes out to make sure it includes:
- All charges that can be legitimately supported by the clinical data (so your organization is fully compensated and doesn’t leave money lying on the table)
- All the information needed to support every included charge (to prevent payment denials and delays)
Many of our most successful customers have learned that this process—which has been perfected under the fee-for-service model for decades—can be “reformulated” for the value-based world and applied to building a concurrent HCC coding process.
And it’s likely that your organization can do the same.
Value-based and fee-for-service processing: different but the same
By now you probably understand that value-based care and fee-for-service are very different reimbursement models. But it’s also important to understand their similarities.
In the fee-for-service world, your revenue cycle management team uses its expertise, processes, and technological tools to “translate” the clinical data in your EMR into the “language” of your payers. They know how to do that by fine-tuning the diagnosis and procedure codes to get them into a correct, payer-ready state. They know which services should be billed individually and which should be billed as bundles. They understand how to handle global periods, and the diagnosis rules around Code First and Code Also.
Under value-based contracts, the details are different, but the clinical data in the EMR still needs to be “translated” into the “language” of the payer. That language consists of HCC codes—which the payer then uses to calculate your patients’ RAF scores, which in turn determine the revenue your organization receives.
The process your RCM team follows to develop, review, and submit fee-for-service claims is basically the same one needed to convert clinical data into HCC codes, verify and correct them to make sure that they’re sufficiently accurate and specific to reflect the actual state of each patient’s health, and submit them to the payer:
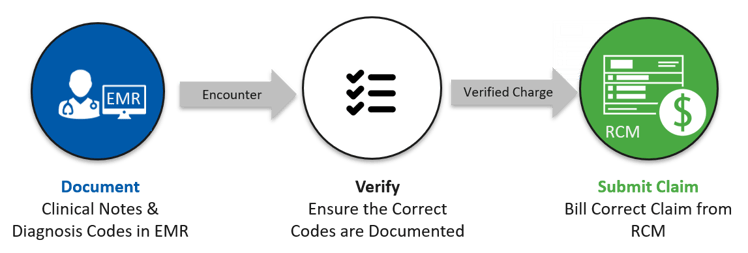
The mindset is the same, too. Your RCM team has been looking at clinical data through a financial lens—and using it to ensure that your organization receives all the revenue it’s entitled to—for years.
A few tips for “reformulating” your RCM assets to improve HCC coding performance
To take your organization’s strong claim production expertise and refocus it on your HCC coding challenge—while taking as much advantage of your existing processes and capabilities as you can—try these suggestions:
- Start small: Your revenue cycle management team is probably organized into smaller, specialized groups. Starting with just one dedicated HCC coder (even part-time!) paired with the right technology will have a huge effect on value-based performance.
- Align with your provider-focused efforts: Just as your organization uses provider-focused efforts around population health and HCC coding awareness to help your clinical team transition to and succeed in value-based care, you can implement revenue-focused initiatives to succeed in value-based reimbursement. Implementing processes that your revenue team has successfully evolved for proven claim review, adapt for your population health team to ensure sufficient value-based reimbursement to care for those patients.
- Take advantage of automation: On the fee-for-service side, your rules engine or claims scrubber improves accuracy, reduces errors, and makes your revenue team more efficient. You’ll find that an HCC coding tool is just as valuable on the value-based side. HCC coding software magnifies the power of your team’s expertise by increasing coder productivity and improving HCC recapture rate, leading to more accurate RAF scores.
Remember, the goal is to develop a workflow that ensures the capture of all properly documented HCC codes before claims submission—which is very similar to the way your revenue cycle team has handled traditional fee-for-service billing issues for years.
You don’t have to re-invent the wheel to financially succeed in value-based care. Start by taking stock of your existing assets and leveraging them to make quick and significant gains.