Denial management in medical billing and coding can be complex, but there are ways to simplify the process. As many as 65% of claim denials are never worked, resulting in an estimated 3% loss of net revenue. For those that are reworked, the average cost to do so is $25, according to the Healthcare Financial Management Association (HFMA).1 By intervening earlier in the revenue cycle management process, you can reduce claim denials and save your organization time and money.
Reduce Claim Denials: Prevent Dirty Data from Entering Your RCM System
With the adoption of EMRs, providers have the added responsibility of entering billing and coding data into the system. While most providers have working billing and coding knowledge, they are by no means experts. Couple that with the ever-changing and complex requirements from payers, and the RCM team is left cleaning up poor billing and coding data. The most efficient revenue cycle teams have found that cleaning this data before it enters the RCM system is key.
Identify and Clean Data on the Front End
Our data shows that an average of 25% of a medical group’s charge volume has administrative coding or billing errors that need correction. Groups who proactively identify these frequently occurring errors and tackle them before charges go into the RCM system reduce claim denials in a meaningful way. By correcting charges earlier in the process, you’re saving your staff time as they no longer need to work denials—the claim meets the payer’s requirements the first time.
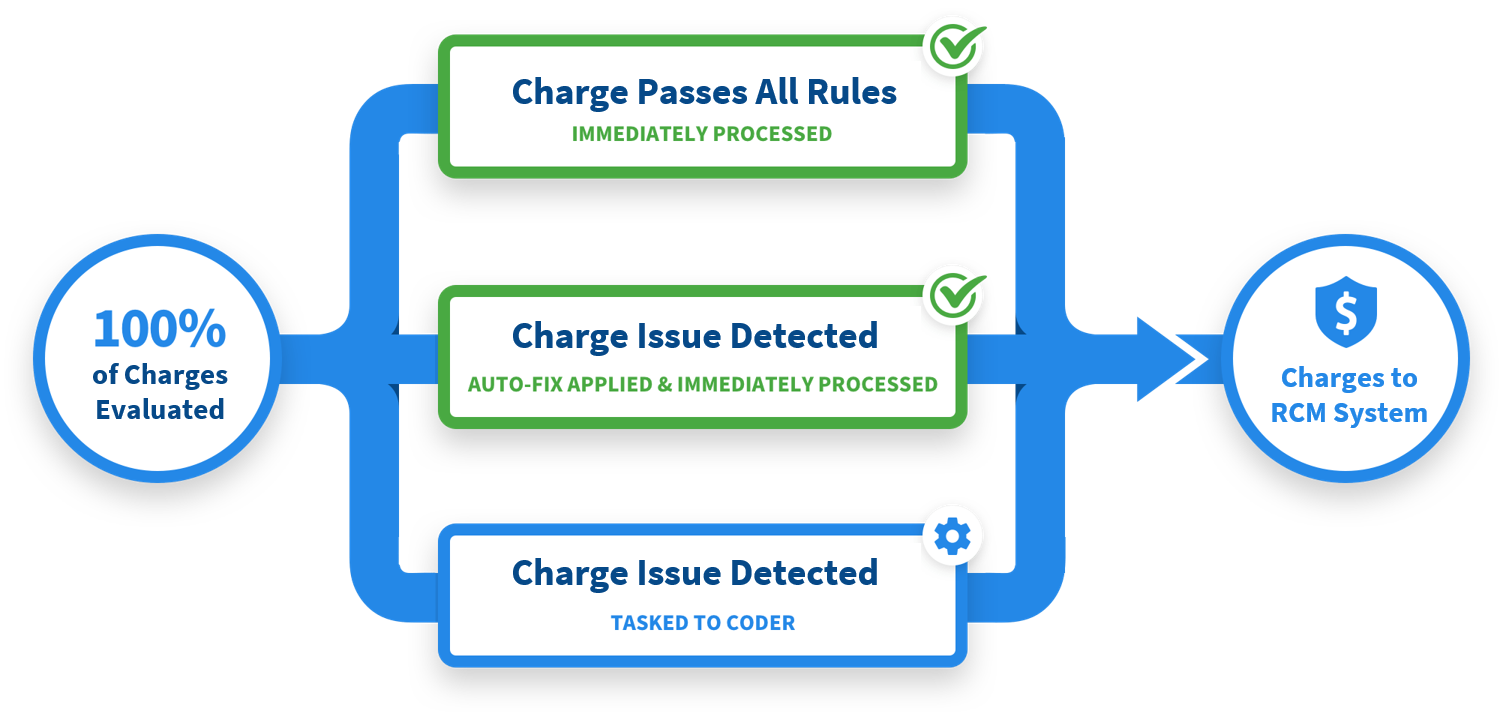
Front-End Automation for Denial Management in Healthcare
RCxRules Revenue Cycle Rules is a medical coding review automation technology that makes the front-end review and correction process seamless. RCxRules Revenue Cycle Rules reviews all charges for coding completeness and accuracy right after entry into your EMR. If a charge is error free it goes directly to the RCM system for claim submission. If an error is detected the technology can either automatically correct the charge (for routine billing and coding errors) or task the error to a coder for further review before going into the RCM system. This exception-based approach maximizes your team’s time, so they spend their valuable time reviewing charges that could cause denials.
RCxRules Revenue Cycle Rules in Action
For a real-world example of how RCxRules Revenue Cycle Rules reduces denials, check out this Case Study featuring Baptist Health. This organization is located in Jacksonville, Florida and has over 150 primary care providers and more than 250 multi-specialty providers. Baptist implemented RCxRules Revenue Cycle software to clean data before it entered the RCM System. This front-end intervention reduced the hours staff spent working on back-end RCM edits by 50% and slashed denials by 12% in just 90 days.
The further upstream you can identify denials, the more time and money you can save overall. Learn how our Revenue Cycle Rules Software and its front-end intervention can help you increase your clean claim rate to reduce claim denials. Set up a 15-minute meeting to learn more.