Completely capturing and documenting Hierarchical Condition Category (HCC) codes for your attributed members is imperative to ensuring accurate risk adjustment scores—and correct and complete payer allocations.
Bring your healthcare organization closer than ever to your full value-based potential with these seven tips:
1. See your patients at least once a year
Diagnoses need to be captured through face-to-face encounters and reported annually. Plan early and create robust outreach plans.
2. Prep for patient visits ahead of time
Help providers identify patients with HCCs ahead of their visits, so activities such as chart prep, problem list reviews, and morning huddles can be made more effective and targeted.
3. Use better forms
To make sure that valid diagnosis codes are documented at the time of the visit, consider options such as Patient Assessment Forms (PAFS) or Comprehensive Health Assessments (CHAs). They’re both designed to aid in the capture of complete and accurate diagnoses at the point of care.
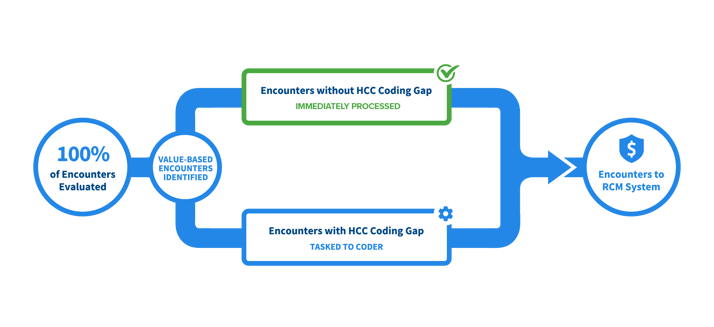
4. Automate the chart review process
Use technology to automatically identify high-value encounters requiring coder review, streamline your workflow, and ensure that HCC coding is completed prior to claim submission.
5. Have the right team in place.
Ensure that your providers are getting all the support they need to complete the proper documentation and capture of HCCs. Review the need for new training initiatives to improve your employees’ knowledge and skills, as well as the need for specialized automation to help them work smarter, faster, and more efficiently. And, if necessary, look into adding support staff such as HCC coders, nurse navigators, and care coordinators.
6. Identify Success Metrics
Identify the metrics and data that your team should track to ensure success, and implement timely, robust reporting on key drivers that impact payments, such as:
-
-
HCC recapture rate (by location and provider)
-
Trending of patient risk adjustment scores
-
Patients with chronic conditions that need to be scheduled
-
Organizations should understand the value of captured HCCs, and evaluate where they’re doing well with capture and where they're falling short. By continually monitoring your HCC performance, and identifying and acting on opportunities for improvement, you can make rapid progress in closing HCC gaps and ensuring complete HCC code capture.
7. Give your providers regular feedback
It’s important to educate providers on their performance in capturing HCCs—and on ways to improve. Work with them to develop strategies to achieve your organization’s capture rate goals.